The crude mortality rate (CMR) is one of the most widely used indicators at MSF and the humanitarian sector more generally, when evaluating the severity of a health crisis within a given population.
It is widely recognised that a CMR equal to or greater than one death per 10,000 persons a day signifies an emergency situation requiring an immediate response. However, the use of the standard emergency threshold as “1/10,000/day” is very questionable: it goes against the official recommendations endorsed by humanitarian organisations and ignores the worldwide decline in mortality rates over the last 30 years.
According to the Sphere and the United Nations High Commissioner for Refugees (UNHCR) emergency handbooks, an emergency should be declared when the crude mortality rate among a given population is at least two times greater than its “normal” value. For UNHCR, the normal mortality rate corresponds to the “baseline mortality of the population prior to displacement, or of the population in the host country”, while Sphere considers it to be the “baseline rate documented for the population prior to the disaster”. It is only when “the baseline rate is unknown or of doubtful validity” that UNHCR and Sphere recommend either using the global 1/10,000/day emergency threshold or the regional thresholds calculated for Sub-Sharan Africa, Middle-East and other regions.
When using 1/10,000/day as a gold standard of acceptable mortality, aid organisations follow a relief policy that is both backwards and contrary to their own recommendations.
The choice of the reference value has very concrete consequences for how aid professionals interpret the gravity of a situation. For example, using the emergency threshold of 1 death/10,000/day, MSF epidemiologists estimated that during the first part of 2015, the overall situation of displaced people and residents living in Maiduguri in Northeast Nigeria wasn’t catastrophic - despite the fact that more than one million villagers had recently sought refuge in town to escape the abuses of Boko Haram and the Nigerian army. A retrospective mortality survey conducted on Maiduguri suburbs estimated that the CMR of the resident population was at 0.19/10,000/day, while that of the displaced population was at 0.41/10,000/day. Since both values were “below the emergency threshold level of 1/10000/day defined for the developing countries in Sub-Saharan Africa”, the results were interpreted as reassuring, and were used by MSF headquarters to justify reducing activity starting that December.
This decision was contested by the field teams who considered that, based on their activities and observations, the situation of the displaced population remained in critical condition. In fact, by applying the HCR’s definition of the emergency threshold, one could have concluded that the CMR of the displaced population was above the emergency threshold since it was twice the CMR of the resident population - 0.41/10,000/day and 0.19/10,000/day, respectively. In this case, the field team had reason to disagree with the interpretation of the survey results, which considered it normal that displaced villagers in Maiduguri died at a rate twice as high as their resident neighbours.

The use of the threshold of 1/10,000/day is even more questionable since this standard was set more than 30 years ago. It corresponds to the CMR set forth in 1985 by the US State Department to declare a health emergency in a refugee camp. This threshold was endorsed by the CDC in 1992 based on the following logic: “In many African countries, the daily CMR (extrapolated from published annual rates) is approximately 0.5/10,000/day during non-emergency conditions. In general, health workers should be extremely concerned when crude mortality rates in a displaced population exceed 1/10,000/day.” In other words, the threshold of 1/10,000/day corresponds to double the average mortality rate recorded in Africa in the mid 1980’s.
Since then, average mortality rate in Sub-Saharan African has been halved (from 0.45 to 0.25/10,000/day, according to the World Bank) while the worldwide average mortality scale has significantly fallen to 0.21/10,000/day (see figure). The 1/10,000/day emergency threshold currently corresponds to four times the average mortality rate in Sub-Saharan Africa and five times the global average.
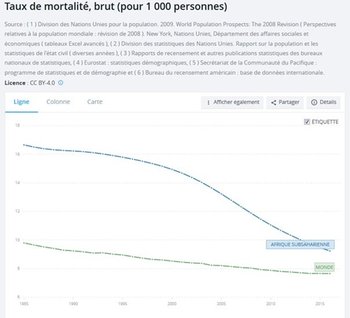
This graph shows the decline of the average mortality rate in Sub-Saharan African (blue) compared to the significant fall of the average mortality rate worldwide (green).
This choice of reference value to qualify emergency situations is highly political, since it determines the level from which we judge the number of deaths to be “excessive” enough to justify exceptional measures. When using 1/10,000/day as a gold standard of acceptable mortality, aid organisations follow a relief policy that is both backwards and contrary to their own recommendations.
Why not round off the global emergency threshold to 0.5/10,000/day?
Perhaps aid actors need a universal emergency benchmark to compare the gravity of different situations. This global emergency threshold should logically correspond to double the “normal mortality” from a statistical point of view, which is to say double the current global average. Since this requires a value that is easy to remember, why not round off the global emergency threshold to 0.5/10,000/day? In any case, redefining the global emergency threshold should not be a barrier to using local emergency thresholds in each specific situation, as it is officially recommended in aid manuals.
This piece was written by Fabrice Weissman in his personal capacity. The opinions expressed in this article are the author's own and do not necessarily reflect the views of MSF-CRASH.